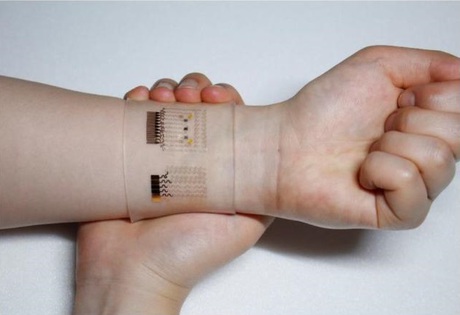
A graphene-based device for diabetes monitoring
Scientists from the Center for Nanoparticle Research at the Institute of Basic Science (IBS) have created a wearable GP-based patch that enables accurate diabetes monitoring and feedback therapy by using human sweat. The team created their biomedical device in response to the need for non-invasive, painless and stress-free monitoring of important markers of diabetes.
Writing in the journal Nature Nanotechnology, the researchers noted that graphene is a versatile material in micro- and macroelectronics due to its high carrier mobility, conductivity, flexibility and optical transparency. However, the low density of electrochemically active defects in graphene synthesised by chemical vapour deposition limits its application in biosensing.
The scientists refined the device’s detecting capabilities by integrating electrochemically active and soft functional materials on a hybrid of gold-doped graphene and a serpentine-shape gold mesh. This was found to improve its electrochemical activity compared to bare graphene and made it sufficient to form a wearable patch.
“The stretchable device features a serpentine bilayer of gold mesh and gold-doped graphene that forms an efficient electrochemical interface for the stable transfer of electrical signals,” the study authors wrote. “The patch consists of a heater, temperature, humidity, glucose and pH sensors and polymeric microneedles that can be thermally activated to deliver drugs transcutaneously.”
The device’s pH and temperature monitoring functions enable systematic corrections of sweat glucose measurements as the enzyme-based glucose sensor is affected by pH (blood acidity levels) and temperature. Study co-author Kim Dae-Hyeong explained, “The patch is applied to the skin, where sweat-based glucose monitoring begins on sweat generation. The humidity sensor monitors the increase in relative humidity (RH).”
It takes an average of 15 minutes for the sweat-uptake layer of the patch to collect sweat and reach an RH over 80%, at which time glucose and pH measurements are initiated. If abnormally high levels of glucose are detected, an insulin-regulating drug is released into the patient’s bloodstream via the microneedles.
The malleable, semitransparent, skin-like appearance of the patch provides easy and comfortable contact with human skin, allowing the sensors to remain unaffected by any skin deformations. This enables stable sensing and efficient drug delivery. The device retains its original sensitivity after multiple uses and used microneedles can be easily replaced with new ones.
“The connection of the device to a portable/wireless power supply and data transmission unit enables the point-of-care treatment of diabetes,” added Dae-Hyeong.
AI-powered wearable turns gestures into robot commands
A new wearable system uses stretchable electronics and artificial intelligence to interpret human...
Graphene-based solar cells power temperature sensors
Researchers have demonstrated the ultra-low-power temperature sensors powered by graphene-based...
3D-printed diamond device powers medical implants
Researchers from RMIT University have developed a 3D-printed diamond–titanium device that...





